Use our convenient online scheduler to book an appointment now.

Epidural Steroid Injection Q & A
- What is the epidural space?
- What causes pain in the epidural space?
- What is an epidural steroid injection?
- What happens during an injection?
- How long does an ESI injection take?
- How will I feel afterwards?
- How long will the relief last?
The space surrounding the dura, which is a protective covering of the spinal cord and its nerves is called the epidural space.
The spine is comprised of 24 vertebrae: 7 in the cervical region, 12 in the thoracic region, and 5 in the lumbar region. Soft discs found between these vertebrae cushion them, hold them together, and control motion.
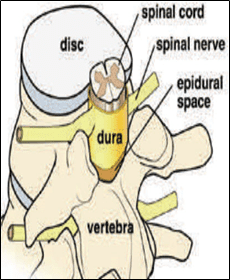
If a disc tears, nucleus pulposus (jelly) inside may leak out. The mechanical pressure from the jelly can inflame nerve roots or the Dura and may cause pain.
Bone spurs called osteophytes can also press against the nerve root, causing pain.
Epidural steroid injections (ESI) are performed to place anti-inflammatory medication (steroids) and local anesthetic/saline in the epidural space to target irritated nerves and reduce pain by reducing inflammation. They are usually performed for patients with spine pain and radiating pain into legs or rams. Injections are performed under x-ray guidance.
There are three different ways to perform a lumbar ESI and your physician will choose the route that offers the best chance of relieving your pain based on several factors. The three methods of ESI are described below:
Caudal ESI: The caudal approach involves an injection at the base of the spine near the tailbone. An advantage of this approach is that it can be performed even if you have had major spine surgery with hardware.
Interlaminar ESI: The interlaminar approach can be performed at all levels of the spine from the low back to the neck. This approach may not be possible if you have had spine surgery in the injection area. An advantage of this approach is that medication maybe delivered closer to the area of pain.
Transforaminal ESI: The transforaminal approach involves placement of the needle into the area where the spinal nerve exits the spine. It can be done throughout the spine but is performed most frequently in the lower back region due to safety concerns in the neck region and mid back region. The approach can be used in areas of prior lumbar surgery and may deliver medication most accurately to the area of nerve root irritation.
A local anesthetic is used to numb your skin. The doctor will then insert a thin needle directly into the epidural space. X-ray guidance is used to ensure the safe and proper position of the needle. A dye may also be injected to ensure correct placement of the needle in the epidural space. When the needle is in the correct position, the doctor will inject the steroid medication mixture.
The injections usually take about 10-15 minutes of total time including positioning the patient, prep and drape and performing the injection. Your procedure may take slightly longer if your physician recommends an approach at two different levels of your spine and or anatomical challenges secondary to factors such as previous surgery, scoliosis, advanced arthritis etc.
The onset of relief from an injection usually takes effects 48-96 hours. Some patients feel improvement sooner and some may take up to 1-2 weeks. There may be a temporarily sensation of pressure at the site of the injection in some cases which usually improves gradually over the next day or so.
Each patient can have a different response to an injection and factors such as extent of severity of mechanical compression, age, biogenetic/pharmacogenetic make up, and prior history of success/lack of success. If a patient does respond favorably to an injection, then the relief can last up to 3 months and sometimes a series of injections must be performed to get the maximum relief depending upon underlying inflammation.
Join our Mailing List
TCO provides patients with orthopedic problems the trusted resources and patient-centered advice they need to “Feel Better. Move Better. Be Better.”
© 2024 Town Center Orthopaedics | All Rights Reserved