Use our convenient online scheduler to book an appointment now.

In a prior post, I discussed what an irreparable rotator cuff tear was and why they can be so problematic. In this post, we will discuss the available treatment options.
As with many other musculoskeletal issues, this problem can sometimes be treated successfully without surgery. Sometimes, however, surgery is needed. Let’s first take a look at the non-operative treatment, and then I will explain the surgical options.
Your Free Guide To Shoulder Injuries, Pain, Treatment & Prevention
Non-surgical Options
As you may recall, these tears rarely are acute injuries and typically occur slowly over time. What makes them irreparable are often the changes that occur to the tendon, its muscle, and the shoulder bones due to the longstanding rotator cuff failure. Often, we don’t know why people with an irreparable rotator cuff tear go from functioning well to functioning so poorly, so abruptly. After all, your rotator cuff often has been torn for years. So what has recently changed?
It may be your pain. It may be inflammation from an injury or overuse. It could also be from swelling that may result from almost any cause. If any of these are the culprit, then correcting the responsible issue may fix your problem…and sometimes it does.
For these patients, trying the non-surgical treatment is reasonable. Usually, this is where we start for most patients. This treatment often includes addressing both pain and dysfunction. Over-the-counter medications and oral anti-inflammatories are used to help with the pain and any inflammation and swelling. Sometimes a cortisone injection is used for these same reasons. As the pain improves, physical therapy can be attempted to improve function and further reduce pain. Although this treatment won’t work on everyone, it can work on some.
Surgical Options
For those in which non-operative treatment is unsuccessful or not a reasonable option, surgery may be helpful. Although the rotator cuff is not completely repairable, there are still surgical options. Let’s take a closer look.
1) Arthroscopic Debridement and/or partial rotator cuff repair
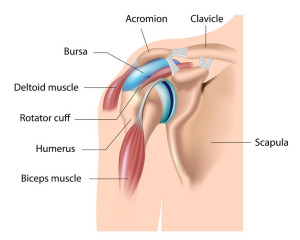
If the primary cause for your symptoms is due to inflammation, bursal swelling, or excessive joint fluid (effusion) arising from inflammation, removing the cause of inflammation may help. Just as washing your eye when it gets inflamed helps reduce eye irritation, washing and cleaning your shoulder joint, potentially could help with shoulder irritation.
How is that done?
This procedure is performed with arthroscopy. Arthroscopy is a minimally invasive procedure that utilizes a fiberoptic camera to look inside a joint, in this case, your shoulder. While doing this, your surgeon can also remove loose particles, inflammation, and excess fluid as well as smooth down rough areas in your shoulder. At the same time, additional problems identified can be addressed. Although your rotator cuff cannot be completely repaired, it is still possible that partially repairing your rotator cuff can stabilize the edges of the rotator cuff, provide some support to your humerus, reduce inflammation and pain, and possibly improve your function. Even though this procedure won’t wholly correct your rotator cuff tear, it may not be the tear or just the tear that’s causing your problem. If not, this procedure could help and may even return you back to how you were before your symptoms started.
2) Superior Capsular Reconstruction
As you may recall, usually with an irreparable superior rotator cuff tear, there is little or no rotator cuff on the top of your humerus. As a result, when you attempt to elevate your arm, you are not engaging your rotator cuff muscles. Still, you are contracting your deltoid, which inserts more distally on your arm than your rotator cuff. As a result, your humerus is pulled upwards. Often this causes the humerus to rise, abutting against the acromion – instead of rotating on the glenoid. Both of these can cause pain and weakness.
Therefore, having something on top of your shoulder in place of the rotator cuff could theoretically prevent this problem. It could enable the humerus to stay centered on and rotate against the glenoid. If so, both your function and pain could improve. Well, one such procedure does exist. This procedure is called a superior capsular reconstruction (SCR).
The procedure…
During an SCR, tissue, either from the patient (autograft) or, more commonly in the US, thick cadaver skin (allograft) is placed arthroscopically and attached to the glenoid and humerus over the shoulder joint. This provides a so-called “reverse trampoline” effect, “which prevents the humeral head from rising while attempting to elevate your shoulder. It also has a secondary benefit of reducing pain, as it acts as a buffer between the humeral head and the acromion.
For this surgery to be effective, your subscapularis, the rotator cuff tendon in the front of the shoulder, must be intact or repaired. There also can’t be very much arthritis in the joint. An SCR won’t directly address arthritic pain, and therefore it is not indicated if the patient has rotator cuff arthropathy.
The recovery from this procedure is similar but slightly slower than that of a rotator cuff repair. So far, results have been favorable, although long-term data is not yet available.
3) Tendon Transfer
Tendon transfers involve releasing one end of a nearby tendon and connecting the released free end of the tendon to the area of your rotator cuff defect, usually to the top of your humerus. These procedures are performed through open incisions and typically involve the tendons of the latissimus dorsi, the trapezius, or the pectoralis major. Tendon transfers tend to result in better improvements in pain rather than function. The overall results of these procedures are not fully understood. The studies evaluating them are small and of more inferior quality, mostly detailing an individual or group of doctors’ experience rather than higher-level statistical analysis. Furthermore, complication rates are high. As a result, these procedures are not commonly used.
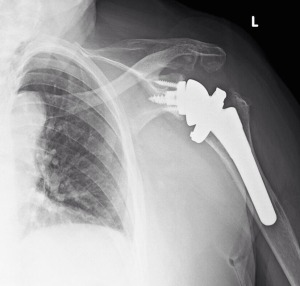
4) Reverse Total Shoulder Replacement
During a reverse shoulder replacement, the shoulder parts are replaced by artificial components, just like in an anatomic or routine shoulder replacement. However, unlike an anatomic shoulder replacement, the implants are reversed from normal anatomy – the ball is placed on the cup side, and the cup is placed on the ball side.
Why is this important?
A standard total shoulder replacement fails early without adequate superior support. In this situation, for reasons already discussed, the humerus rises up when attempting to move your shoulder. This results in premature wear and loosening of the glenoid implant, which leads to early failure of the shoulder replacement.
The reverse shoulder replacement is different. This altered anatomy enables the humerus to rotate when the deltoid pulls, instead of rising up. This allows for improved arm elevation. As a result, when successful, reverse shoulder arthroplasty leads to reduced pain and improved function.
The postop treatment and recovery timeline for a reverse total shoulder replacement is similar to that for a more standard shoulder replacement. Typically this procedure is reserved for patients who have rotator cuff arthropathy or are older with lower shoulder demands.
Possible Future Directions…
Subacromial Balloon Spacer
A newer procedure has recently been developed by an Israeli company. It involves arthroscopically inserting a dissolvable balloon into the subacromial space just above the rotator cuff. Once in place, the balloon is then inflated. Just like the SCR mentioned above, this balloon maintains the space between the humeral head and the acromion. However, with a much simpler and quicker technique. In the US, this technique is not FDA approved. As a result, outside of ongoing clinical trials, this procedure is not yet available in the US.
Early studies have shown that this technique provides short term improvements in pain and function in some of the patients. More information is still needed to determine if this will be an option and, if so, for which patients. I’ll keep my eye on it and let you know as the data unfolds.
Symptomatic irreparable rotator cuff tears can be very troublesome for patients. It is often a source of significant pain and disability. Fortunately, there are treatment options. If you’re having severe pain and problems and you have been told that your rotator cuff is not repairable, see your shoulder specialist. There’s a good chance they can help.
Join our Mailing List
TCO provides patients with orthopedic problems the trusted resources and patient-centered advice they need to “Feel Better. Move Better. Be Better.”
© 2024 Town Center Orthopaedics | All Rights Reserved