Use our convenient online scheduler to book an appointment now.
PRP (Platelet Rich Plasma) is all the rage. But should it be? PRP is a treatment that has been discussed widely in the news and particularly in our sports media. It is a modification of your own blood that is intended to promote healing in slow to heal tissues.
Platelets are one of the three common cell types found in blood. Plasma is the liquid part of our blood. Not only are platelets integral in initiating normal blood clotting, but they also carry important growth factors. These factors are very important in healing following an injury. The theory behind the use of PRP is that if we can concentrate platelets, and therefore these growth factors, and then administer these factors to areas of injury, we can speed up tissue healing.
As a result, PRP has been used in a number of areas in Orthopaedics and Sports Medicine. Primarily, PRP has been used to promote healing in the following musculoskeletal conditions:
PRP Use
- Tendinosis (Degenerative injuries of tendons)
- Muscle strains and ligament sprains
- Surgical recovery
- Arthritis
PRP Efficacy: Fact or Fiction?
There are anecdotal success in all these areas when treated with PRP. Unfortunately, when evaluated in scientific studies, the results of PRP as presently formulated and used, have been disappointing in most of these cases. Why?
PRP: Component and usage variability
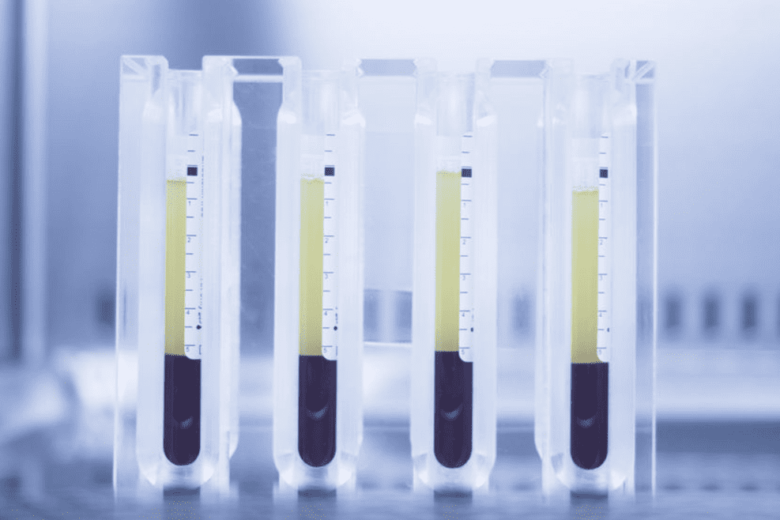
Well, it’s been found that one formulation of PRP differs from another, even when the specimen is taken from the same person…even minutes apart. Typically a sample of your blood is drawn. This specimen is then mixed with other compounds to prevent clotting and to “activate” the critical cells. The sample is then placed in a centrifuge that spins at various speeds and for a given time period. This rapid spinning separates the components of blood based on size and weight. As a result, the platelet rich plasma layer is seperated from the other components. This is the PRP. Although this process sounds very scientific, it really is not. There is no universally agreed upon centrifuge speed, spinning time or agreement as to what other components to mix in with the specimen. In essence, we are not all using “apples”. Some are using “oranges”. So comparing results is difficult.
Once the specimen is isolated, it is injected into the area of injury. This can be done in your doctor’s office. Some perform this with ultrasound guidance to increase the accuracy of placement, others don’t. Surprisingly, there is also no agreement as to how large the sample needs to be, how often it needs to be given, what the interim between treatments should be and what to do after the treatment. More “apples” and “oranges” .
PRP: Simplicity in a complex environment
Furthermore, our understanding of the complexity of healing is rather immature. This process is likely much more complex than simply placing growth factors in an area and expecting them to do their magic. We know that they need to be activated, we just don’t know how. How many people work without getting paid? Well we don’t know what these cells like to be paid or how much they expect to get paid before they begin to work. Finally, it is very likely other cells are needed to promote and sustain the affect of these growth factors…but we don’t know which ones. We are playing football with a team of only quarterbacks…we need some lineman…and others.
PRP: Some promise
As a result of these reasons and additional ones, the overall success of PRP has not been as good as initial expectations. With that said, there are some areas where promise has been seen. These are:
- Tendinosis of the elbow (tennis elbow) and potentially of the knee (patellar tendinosis)
- Arthritis
Even in these cases however, curing the problem has not been reliably seen when treating tendinosis and never seen when used in the treatment of arthritis. Improving symptoms is more likely, but still far from universal.
There likely is something to PRP but we are clearly in the very early stages of our understanding. Over time, PRP may become a wonderful and revolutionary treatment option…or it may fall to the waste-side like so many other initially promising treatments. Time will tell.
This is a very interesting topic and likely to become more interesting with time. For now, if you would like more information, view Dr. Howard Luks and myself as we discuss PRP in our 3rd installment of our video series – The Two Boneheads.
Once again, if you have any questions, pass them along. We’d love to hear from you.
Join our Mailing List
TCO provides patients with orthopedic problems the trusted resources and patient-centered advice they need to “Feel Better. Move Better. Be Better.”
© 2024 Town Center Orthopaedics | All Rights Reserved


